Table of contents
1. When Period Pain Feels More Than ‘Just Cramps’
2. Hormonal Imbalance and Period Pain: Estrogen, Testosterone and Prostaglandins
3. When Your Pain Could Be Endo In Disguise
4. Delayed Diagnoses: A Real Pain
5. Daye’s Period and Pelvic Pain Clinic & At-Home Hormone Testing
6. Trust Your Symptoms: They’re Trying To Tell You Something
Written by Etienne Paddy
Medically reviewed by Sarah Montagu (RN DFSRH, BSc)
Illustrated by Valko Slavov Maria Papazova
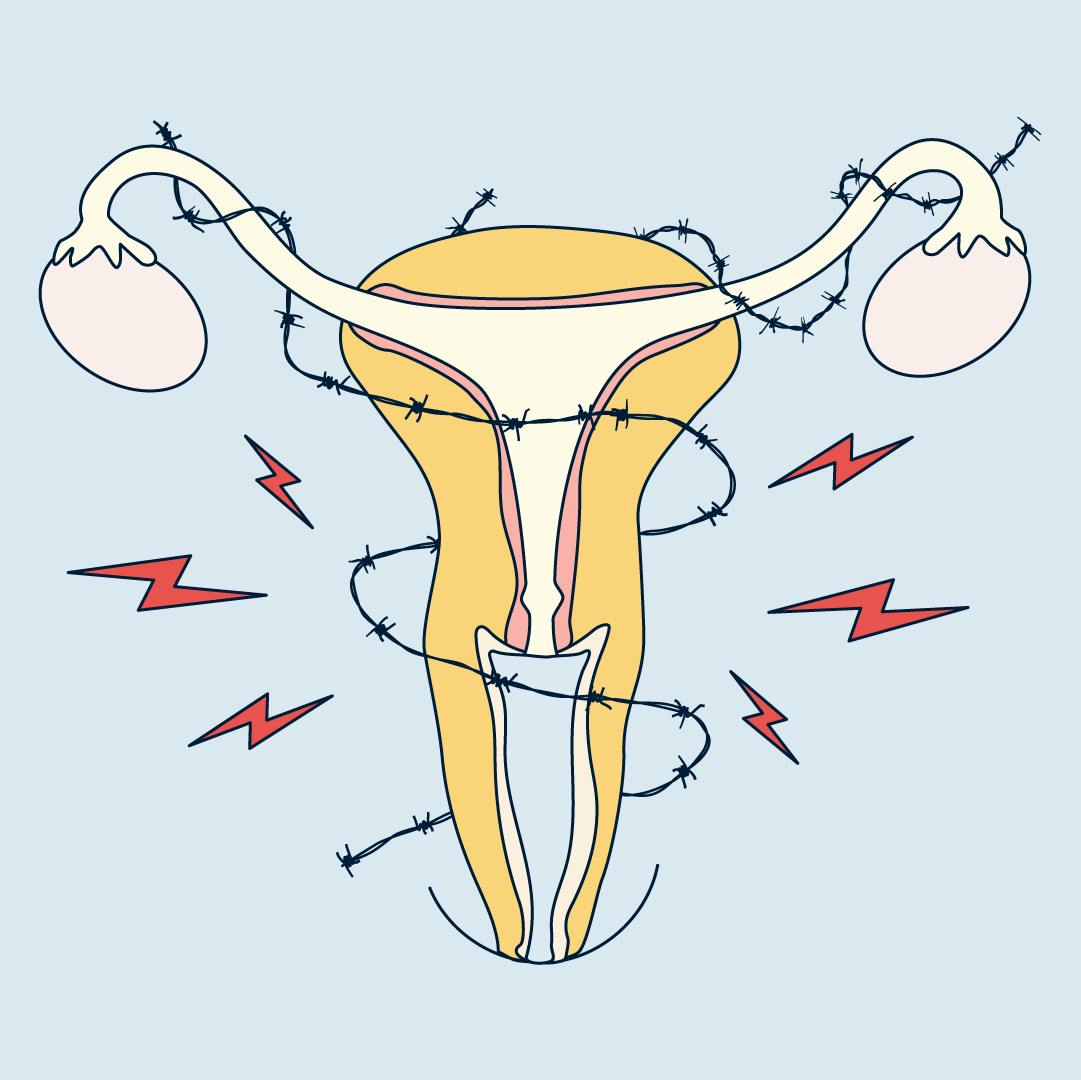
When Period Pain Feels More Than ‘Just Cramps’
Ever suffered a period that had you doubled over, white knuckled, wondering how everybody else does it? Your friends need a hot water bottle when their time comes, but you need a whole week off.
How are other people functioning each month while your period feels like a uterus full of razorblades and you're being used as a human maraca?
Far too many women accept extreme period pain because society has conditioned us to. Our bodies are complicated and there’s no one-size-fits-all solution to this invisible, yet very real problem. Decades of research has routinely left people with periods out of the picture, resulting in limited treatment options and a total lack of awareness of how bad it can really get.
And so, period pain is so often dismissed as something to just ‘deal with’, part of the package of having a uterus. It makes me wonder, if everyone (including men) had it that bad, would period pain be a thing of the past?
It’s important to have these conversations, because pain should not be ignored. Extreme period pain can be a signal from your body. A neon sign telling you that your hormones are out of balance—or, maybe, that something deeper like endometriosis is at play.
When your pain becomes debilitating, it’s time to ask questions. And your hormones might just hold the answers.
Hormonal Imbalance and Period Pain: Oestrogen, Testosterone and Prostaglandins
If your period is your body’s monthly performance, oestrogen and progesterone are the lead singers. When they’re in harmony? Smooth set. When the balance tips…things get painful.
How Hormones Shape Your Cycle—And Your Pain.
During a typical menstrual cycle, oestrogen helps build up the uterine lining, while progesterone works to stabilise it. As the cycle nears its end, both hormones drop sharply, and this hormonal dip is what triggers the release of prostaglandins.
Prostaglandins are hormone-like substances that tell the uterus to contract. These help remove the uterine lining (aka your period), but they also cause that pain we’re all such big fans of. (Psst—check out this blog post for ways to manage period cramps).
The higher your prostaglandin levels, the more intense the cramps.
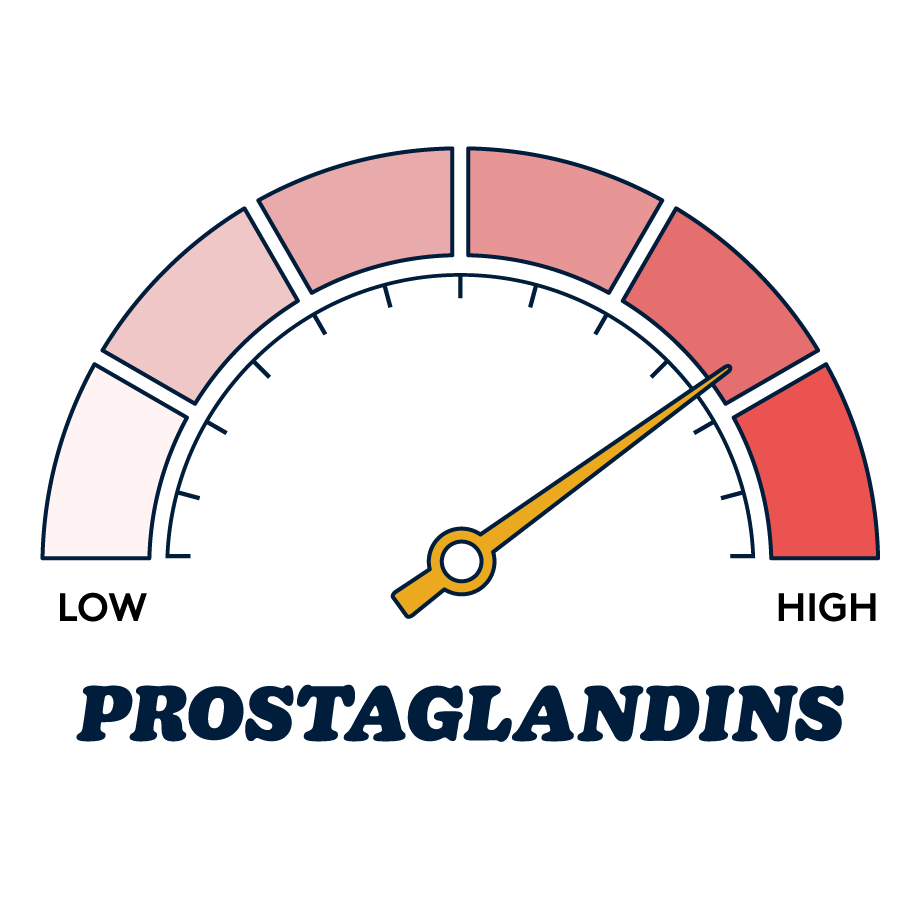
And again, in a typical menstrual cycle, progesterone usually helps keep inflammation down. During the second half of the menstrual cycle (after ovulation), it works like a calming agent. After ovulation, the body starts to store fatty acids, like omega-6 and arachidonic acid, in the walls of the cells. And these fatty acids stay put—until your progesterone levels drop. And that’s when they’re released and used to make pro-inflammatory chemicals, like prostaglandins.
So, when your progesterone levels are low to start with…there’s less hormone holding those fatty acids at bay. Now, they can run unchecked and make more of those cramp-inducing prostaglandins.
Testosterone may also play a role too. Although often overlooked in female health, it has been shown to have an impact on pain sensitivity. One study found that “variability in testosterone (and to a lesser degree estradiol) was associated with pain; testosterone was antinociceptive, whereas estradiol was pronociceptive” (Bartley et al., 2015). This basically means that these scientists found that testosterone helped reduce pain sensitivity, where estradiol (a type of estrogen) tended to increase it.
So, reduced testosterone could possibly make already painful periods feel even worse. However, more research is needed to fully understand this relationship in the context of menstrual pain.
TL;DR: Too much oestrogen + too little progesterone + low testosterone = more inflammation, more uterine contractions and way more pain than most people realise is possible.
So where does endometriosis come in?
Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus, which can really disrupt your hormonal balance. It’s strongly associated with oestrogen dominance and progesterone deficiency, but in a way that’s persistent, chronic, and harder to manage than the usual hormonal ups and downs many people experience.
Oestrogen doesn’t just help build tissue—it can actually encourage these misplaced patches of tissue to grow. Without enough progesterone to help keep things calm, inflammation can build up and become really uncomfortable.
Hormonal imbalances on their own can be tough to deal with, but with endometriosis, the inflammation and pain often feel much more intense. So, it can be especially disheartening to struggle with this extreme pain and have it dismissed as part of the uterus-ownership deal.
Now, we’re not interested in scaremongering at all. A hormonal imbalance does not, by any means, diagnose you with endometriosis. Rather, it can be an important sign to pay attention to—especially when the pain is severe, long-lasting, and comes with other symptoms.
It’s something that’s absolutely worth exploring with your healthcare provider to get the support and answers you deserve.
When Your Pain Could Be Endo In Disguise
Symptoms to look out for:
- Chronic pelvic pain (not just around your period)
- Pain during sex
- Fatigue
- Heavy or irregular menstrual bleeding
- Infertility or difficulty conceiving
- Bowel/bladder issues
These symptoms often overlap with other conditions, like IBS or pelvic inflammatory disease, making diagnosis tricky—and delayed.
Which, if you’ve ever tried to get an endometriosis diagnosis, you’ll know is the very last thing you want.
Delayed Diagnoses: A Real Pain
If you’ve ever taken a scroll through r/Endo, you’ll see a community of resilience and frustration. Many share stories of waiting years (sometimes nearly a whole decade!) for a diagnosis. Too often they’ve been dismissed by doctors, told their pain was “normal” or misdiagnosed with IBS, anxiety or simply stress. This isn’t just frustrating, it’s heartbreaking. Because the pain is real and life-altering.
What makes endometriosis particularly tricky is that many cases start with mild or irregular symptoms, often chalked up to hormone fluctuations, period cramps or stress related issues. But, as we learned, endometriosis can hide beneath that, quietly worsening, causing deeper inflammation, pain and even affecting fertility.
The average diagnostic delay for endometriosis is a staggering 8 years, 10 months, even though it’s the second most common gynaecological condition in the UK. This delay accounts for years of uncertainty, missed opportunities for early treatment and so much unnecessary suffering.
Users report being told “it could be worse, you could be paralysed”. One story details how years elapsed while a patient went to five gynaecologists who each said they were ‘fine’ (when they ‘couldn’t function at all’) to finally find that their hunch had been right all along and endometriosis was, in fact, the cause of their pain.
On r/Endo, you’ll not only find stories of people struggling with endometriosis, but also a powerhouse of community support. People share their journeys, tips for managing pain, navigating the healthcare system and coping with the emotional toll. It’s a safe space, whether you’re newly diagnosed, still searching for answers or have been a long-term endo warrior. Because—remember this!—you are not alone.
Unfortunately, many people face barriers like being dismissed or not having easy access to the care they need, and no one should have to endure years of debilitating pain because of that.
And that’s why we do what we do.
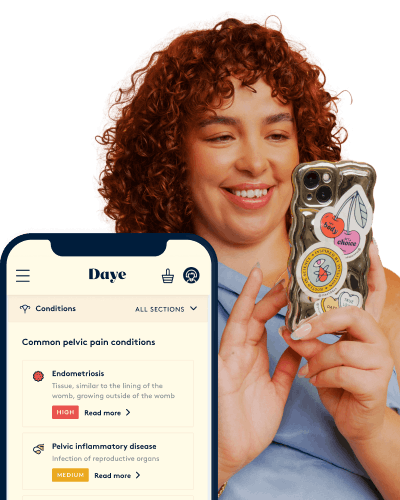
Daye’s Period and Pelvic Pain Clinic & At-Home Hormone Testing
At our Period & Pelvic Pain Clinic, long waits and dismissive diagnoses are a thing of the past. We’re replacing inconvenience with innovation that helps you get to the bottom of, well, you. Consider this your first step to make sense of your symptoms.
If you're wondering whether your period pain could be linked to a hormone imbalance or endometriosis, we also offer hormone testing to help unearth the root cause of your pain in a comprehensive approach to fast-track diagnosis.
Understanding your hormone levels helps you identify how deeply they’re influencing your symptoms, opening up pathways to restore balance and feel better.
Trust Your Symptoms: They’re Trying To Tell You Something
If you’re dealing with debilitating period pain, don’t brush it off. Hormone imbalances like oestrogen dominance and progesterone deficiency could be vital clues—and potentially a red flag for endometriosis.
Start by tracking your symptoms. Talk to your healthcare provider. Or better yet, explore your symptoms through Daye’s Period & Pelvic Pain Clinic. Because early insights lead to early answers. Let’s get smart with science—and compassionate with ourselves.
Your pain is real. Your symptoms matter. And answers could be closer than you think.
Fill out our period pain questionnaire to get started.
Take the pain out of your period
90% of us experience period pain, and when left unmanaged it leads to us losing 150 million productive work days per year.
Mentioned Products