Table of contents
1. Polycystic ovary syndrome (PCOS) is a group of symptoms that affects the function of ovaries and ovulation. It also impacts someone’s physical and mental health.
2. What does PCOS mean?
3. What causes PCOS?
4. Common symptoms of PCOS
5. PCOS and pregnancy
6. Can PCOS be cured?
7. How PCOS is treated?
8. What happens if you don’t treat PCOS?
Written by Liv Cassano
Illustrated by Sabrina Bezerra
Polycystic ovary syndrome (PCOS) is a group of symptoms that affects the function of ovaries and ovulation. It also impacts someone’s physical and mental health.
PCOS presents itself through 3 main features: irregular periods, a higher level of androgens, and polycystic ovaries. In order to be diagnosed with PCOS, you need to have at least 2 of these features (not everyone with PCOS will have all 3).
What does PCOS mean?
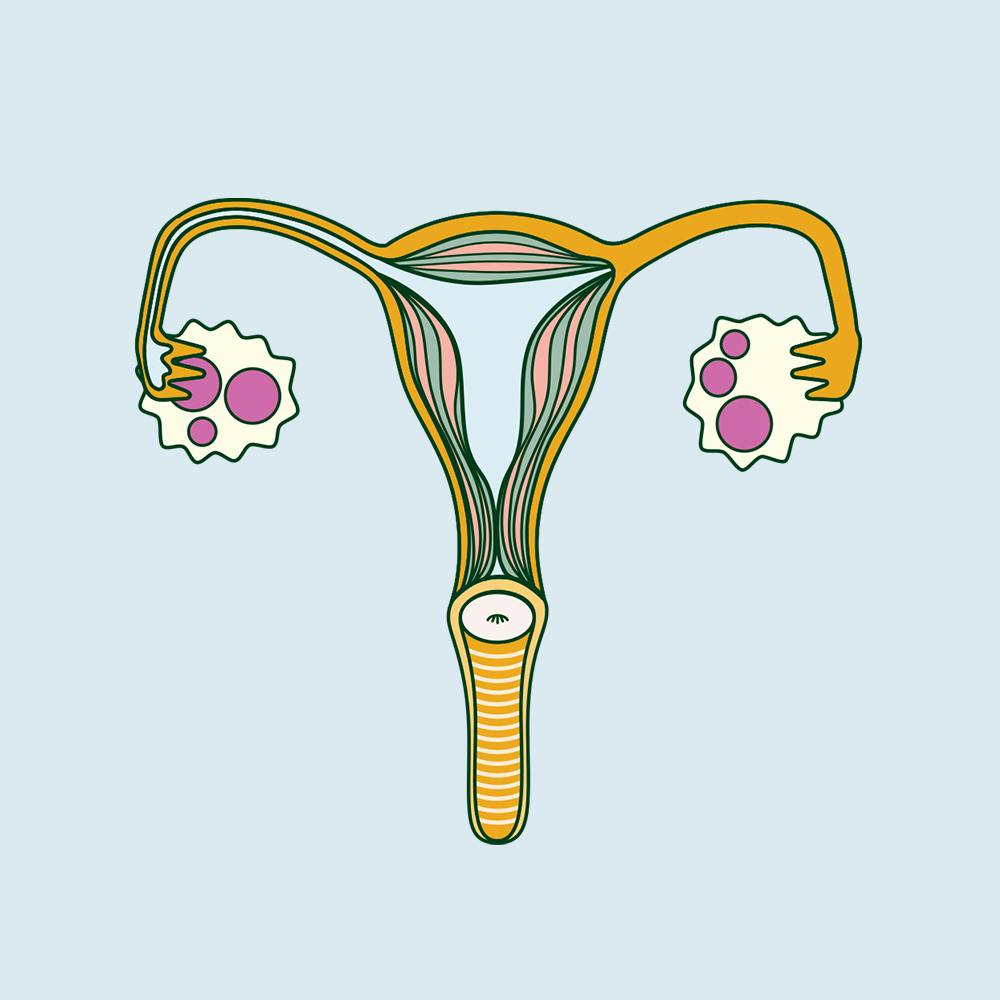
When your ovaries are getting ready to release an egg, they develop small fluid-filled sacs (follicles) that start to develop an egg for fertilisation. One of these follicles eventually releases the egg (ovulation). In some people with PCOS, follicles don’t fully mature or release an egg, so these follicles remain on their ovaries (usually 10 or more) .
Despite the name, cysts in polycystic ovaries aren’t always present in women and AFAB individuals with PCOS. When they are present, they’re not like the cysts you’d get in other parts of your body. Rather, they’re follicles that never matured and contain an underdeveloped egg.
It was originally thought that these follicular cysts were the cause of PCOS (rather than a common symptom), and due to the confusion over the name of the condition, the healthcare community has been considering changing the name.
Take the pain out of your period
90% of us experience period pain, and when left unmanaged it leads to us losing 150 million productive work days per year.
What causes PCOS?
Doctors still haven’t figured out the precise cause of PCOS, but the main theory is that PCOS is caused by a hormone imbalance.
Many people with PCOS have higher levels of testosterone (often referred to as the “male hormone,” but naturally produced by the ovaries as well). They also have higher levels of luteinising hormone (LH), which stimulates ovulation but can have undesired effects if it’s too high, as well as lower levels of sex hormone-binding globulin (SHBG), a protein that binds to testosterone and reduces its effects.
The exact reason for this hormone imbalance is unknown, but it’s thought to either originate directly from the ovaries (which don’t function properly due to hormone production), or from insulin resistance.
Higher levels of insulin and/or LH can also cause your ovaries to produce more testosterone, which interferes with follicle development and stops normal ovulation.
Is polycystic ovarian syndrome genetic?
PCOS also sometimes runs in families, which suggests that there may be a genetic component to PCOS. However, specific genes associated with PCOS haven’t been discovered yet.
Common symptoms of PCOS
PCOC is a common condition and it’s estimated that around 1 in 10 women and AFAB individuals in the UK have PCOS. Of those, half don’t show any symptoms, which means PCOS is often undiagnosed, making it hard to know precisely how many people suffer from it.
If you do have symptoms of PCOS, they'll typically appear during your late teens or early 20s and include:
- irregular periods or no periods at all (amenorrhea)
- difficulty getting pregnant
- excessive body and facial hair, thinning hair or baldness
- weight gain
- acne
PCOS and hair growth
Higher levels of testosterone prevent normal ovulation, causing the formation of follicular cysts and irregular periods, as well as excess body and facial hair.
PCOS and diabetes
You may be familiar with insulin’s role in diabetes, but it plays a role in PCOS as well. Insulin is a hormone produced in the pancreas that regulates blood sugar levels. It helps glucose (sugar) move from the blood to cells, where it’s broken down to produce energy.
High levels of insulin can cause weight gain and excess body fat can in turn produce more insulin, increasing the risk of developing type 2 diabetes as well as higher levels of cholesterol. If someone has insulin resistance, their cells are less receptive to insulin so their body produces more of it to compensate.
Insulin resistance and PCOS can be mutually exclusive, but the two conditions are related, and 70% of PCOS sufferers are insulin resistant. Studies have determined that a person with polycystic ovarian syndrome has a much higher risk of developing type 2 diabetes.
PCOS and pregnancy
For those trying to get pregnant, certain medications can increase your chances of conceiving. Guidelines are evolving for fertility treatment in PCOS patients, but the medication clomifene (also known as clomiphene) is often prescribed to stimulate ovulation, as is letrozole (which has just been added as first-line management for subfertility due to PCOS).
A recently published study showed that although it takes longer for people with PCOS to conceive, the overall chances of having a baby is the same as people without PCOS (when the condition is diagnosed and treated).
Can PCOS be cured?
Due to the mystery surrounding PCOS, treatment and management varies greatly from person to person and largely depends on symptoms. While there is currently no cure-all for PCOS, a wide range of treatments can help minimise symptoms.
How PCOS is treated?
Since the exact cause of PCOS is unknown, currently there is no cure, nor is there one sole treatment. However, there are different treatments available to manage symptoms and prevent complications.
If you’ve been diagnosed with PCOS, your doctor will likely prescribe a series of blood tests to check for high cholesterol or hormone imbalances, as well as an ultrasound scan to check for polycystic ovaries.
Weight management
The first course of action for PCOS is usually (albeit frustratingly) weight management. As weight gain and excess body fat are a symptom of PCOS that can make the condition worse, doctors often recommend good nutrition and exercise as a way to manage symptoms.
The advice of losing weight is often a problematic one (and it can be triggering for anyone suffering or recovering from eating disorders), but there are other ways to treat PCOS.
Hormonal contraception
Although there is no treatment specifically aimed at balancing hormones, several forms of hormonal contraception can offset PCOS symptoms. The combined oral contraceptive pill (COCP), contraceptive patch and vaginal ring have been shown to improve acne and excess hair growth, as well as make periods more regular.
Diabetes management
In addition to weight loss management, metformin is prescribed to lower insulin and blood sugar levels in insulin-resistant PCOS sufferers.
Hysterectomy
For people with severe PCOS or a serious risk of ovarian cancer, a hysterectomy is an option. The ovaries will be removed, thus removing further cystic growth. This also removes the chance of being pregnant in the future, so it is a serious health decision to make.
What happens if you don’t treat PCOS?
In addition to an increased risk of diabetes, high cholesterol, and infertility, untreated PCOS has been linked to a host of other serious conditions, including cardiovascular disease and endometrial, ovarian and breast cancers.
TL;DR
- Polycystic ovary syndrome (PCOS) i affects normal ovarian function and ovulation. In order to be diagnosed, you need to have 2 out of the following 3: a higher levels of androgens, irregular periods and polycystic ovaries.
- Despite what the name may suggest, polycystic ovaries aren’t a prerequisite for PCOS. Unlike cysts you’d find elsewhere on your body, they’re follicles that never matured and contain an undeveloped egg.
- PCOS causes irregular periods, excessive hair growth, difficulty conceiving, weight gain and acne. It’s also linked to depression and anxiety.
- Insulin resistance and genetics are both possible causes for excess testosterone, which stop ovaries from functioning properly and releasing an egg every month (ovulation).
- There is no cure for PCOS aside from hysterectomy, nor is there one single treatment. However, there are several treatments aimed at managing individual symptoms. These include some forms of hormonal contraception, certain medications and general lifestyle changes like good nutrition and exercise.