Table of contents
1. Cortisol 101: What it does and why it matters
2. How does high cortisol affect my cycle?
3. How do I spot high cortisol?
4. Missing signs & misdiagnosis
5. The problem with standard cortisol testing
6. Cortisol and your long-term health
7. No, you don’t need a cortisol detox
8. Need answers? Daye can help
Written by Eleanor Riches
Medically reviewed by Sarah Montagu (RN DFSRH, BSc)
Illustrated by Valko Slavov
You’ve probably seen cortisol all over socials, framed as the “belly fat hormone” or the reason you’re always tired. But beyond buzzwords and detox powders, there’s a deeper story.
Cortisol is your body’s main stress hormone; it’s essential for daily function. But when stress becomes chronic, high cortisol levels can start to mess with more than your mood and energy – it can throw your whole hormonal rhythm out of sync.
Here’s what the science says about the real connection between stress, hormones and your health, and what you can do about it.
Cortisol 101: What it does and why it matters
Cortisol is your body’s main stress hormone, but that doesn’t make it the enemy. It’s actually essential for everyday functioning.
Cortisol helps you:
- Wake up and feel alert in the morning
- Stay energised and focused
- Bounce back from illness and injury
- Handle stress and pressure
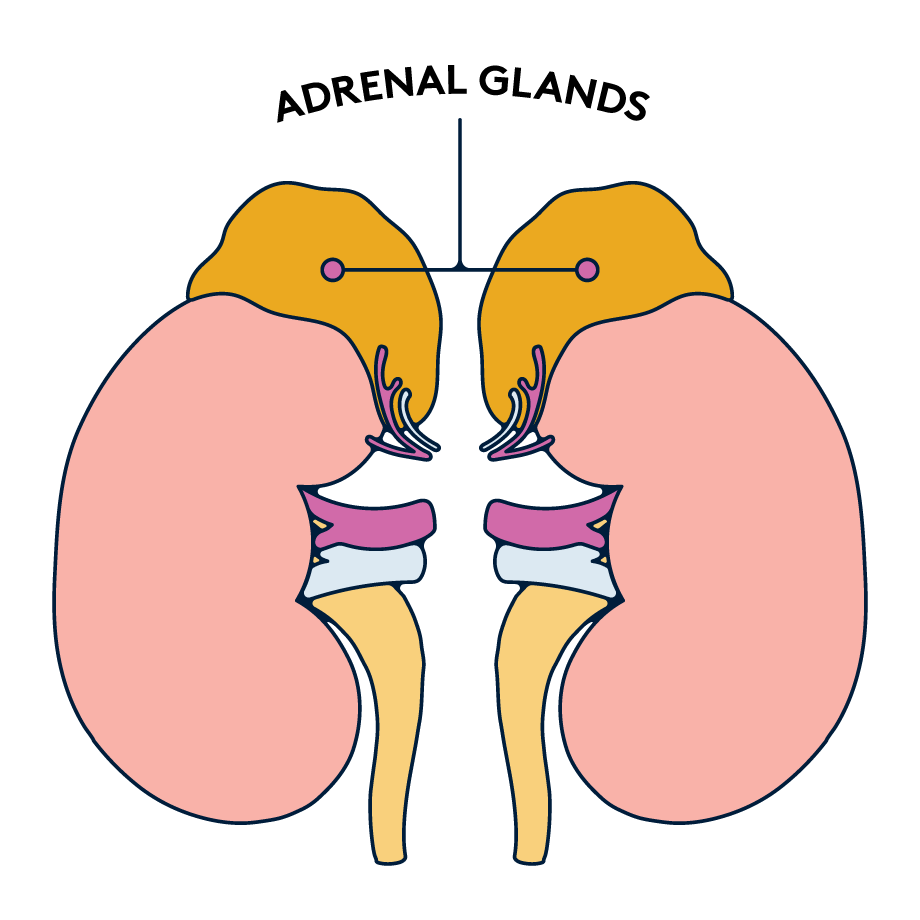
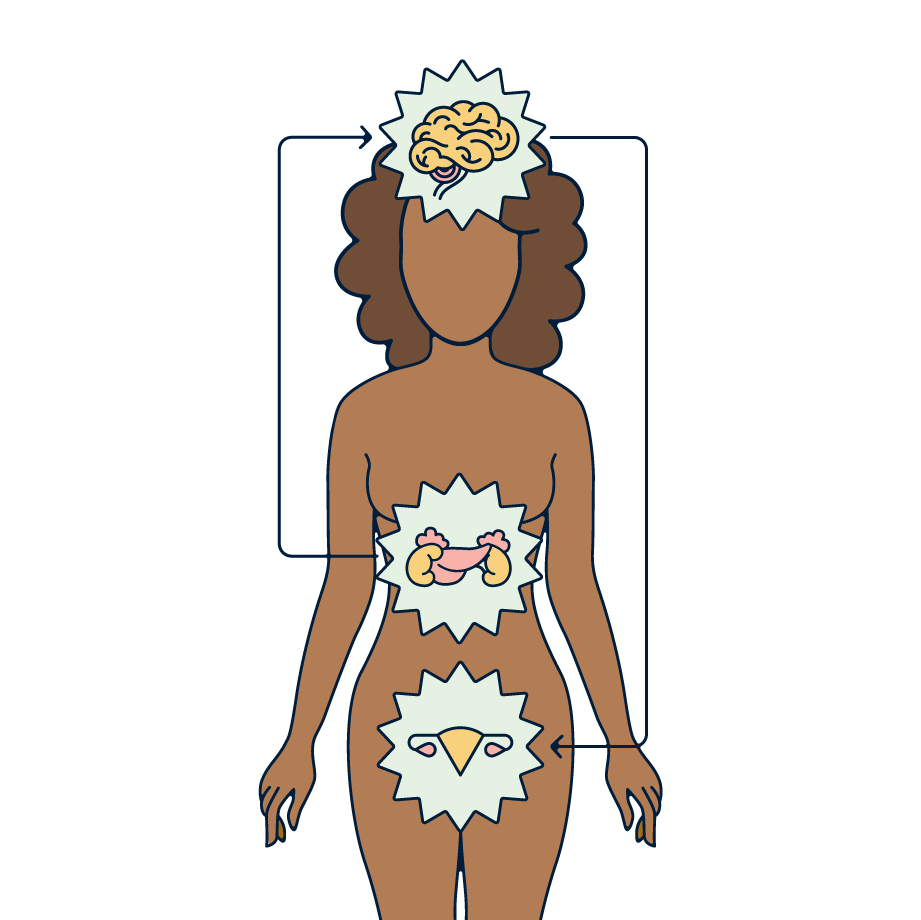
Cortisol is made by your adrenal glands (small glands that sit on top of your kidneys). It’s controlled by the HPA axis (hypothalamic-pituitary-adrenal axis) – a communication loop between your brain and adrenal glands that helps you respond to stress.
But cortisol doesn’t work alone.
Your HPA axis is tightly connected to your HPO axis (hypothalamic-pituitary-ovarian axis), the system that controls your reproductive hormones. They’re super responsive to each other. When your body’s in a constant state of stress, your cortisol levels stay high, and this connection gets disrupted.
How does high cortisol affect my cycle?
You don’t need to be completely burnt out for stress to mess with your cycle. Even low-level, ongoing pressure can quietly impact your hormones over time.
When cortisol levels stay high for too long, it interferes with the signals your brain sends to your ovaries. This can:
- Delay or suppress ovulation
- Reduce progesterone production
- Disrupt your cycle’s rhythm
This isn’t a flaw, it’s a built-in survival response. When stress takes over, your body puts reproduction on pause. And if that stress becomes constant, your body might struggle to find its rhythm again.
You might notice:
- Your period comes late, or not at all
- Ovulation is hard to track or unpredictable
- The second half of your cycle (the luteal phase) is shorter
- Your period is heavier, more painful, or just feels different
Some research links chronic stress to fertility challenges, lower IVF success and poorer egg quality. Stress can also affect gonadotropin-releasing hormone (GnRH), the brain’s signal to trigger FSH and LH production, which are key for making ovulation happen.
However, it’s important to note that stress is complex and difficult to measure, so the research is still limited. Cortisol levels alone aren’t enough to predict your fertility; it needs to be factored into the bigger picture.
How do I spot high cortisol?
Not all stress shows up in panic attacks or breakdowns. Cortisol imbalance is often subtle and flies under the radar.
Common signs include:
- Low energy, especially in the morning or after meals
- Poor sleep or feeling “wired but tired”
- Irregular or missing periods
- Low libido or mood swings
- Brain fog and forgetfulness
- Unexplained weight gain, especially around the belly
If your symptoms are persistent, vague, or hard to explain, don’t rule out cortisol. Your body might be waving a red flag.
Missing signs & misdiagnosis
Cortisol imbalance is easy to miss, and even easier to mislabel. Symptoms can overlap with common conditions like anxiety, PCOS, thyroid issues and perimenopause, making it difficult to spot.
On Reddit, women share stories of feeling “off” for years; dealing with unpredictable cycles, crashing energy and stubborn weight gain, only to discover that cortisol was part of the puzzle. Many seek advice on lowering cortisol (especially those with PCOS), while others are sceptical of the cortisol wellness hype.
A few also discuss Cushing’s syndrome, a rare condition caused by chronically high cortisol. Symptoms like purple stretch marks, thinning skin and high blood pressure are often misread. There’s also confusion around diagnosis criteria, making it difficult to get a formal diagnosis.
That’s exactly why self-advocacy matters. When your symptoms don’t add up, keep asking questions. Remember: you know your body better than anyone.
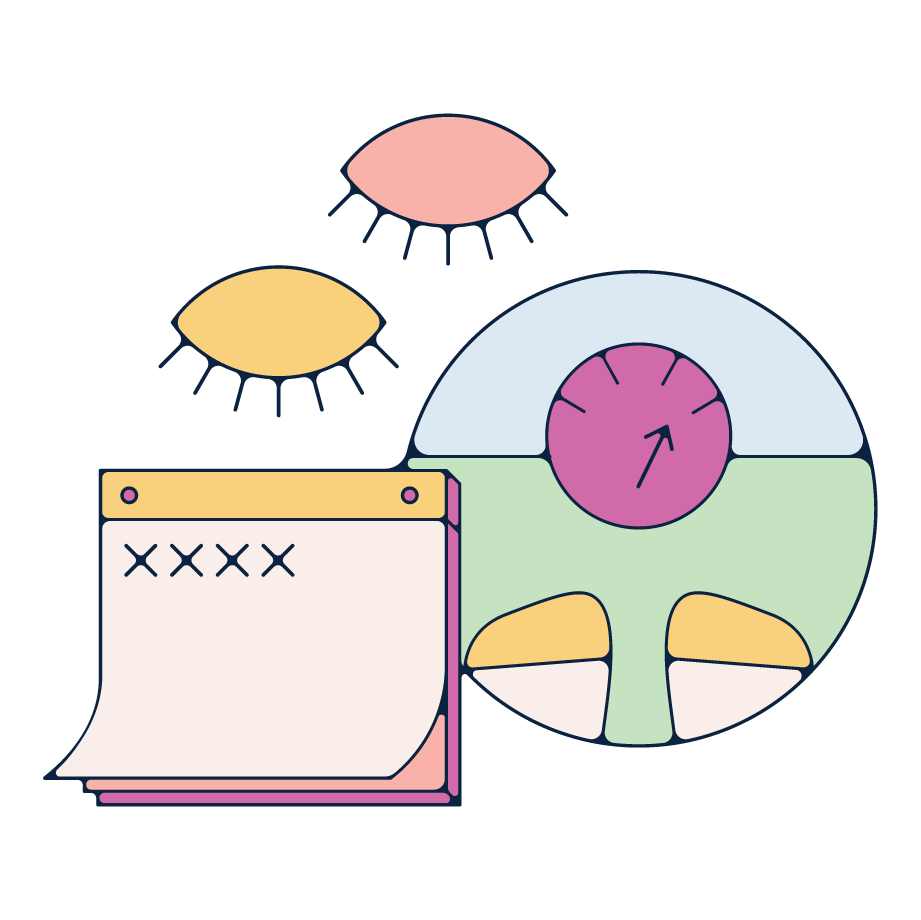
The problem with standard cortisol testing
Cortisol isn’t constant. It follows a daily rhythm, rising in the morning to help wake you up, then gradually dropping so you can wind down at night. That’s why a single blood test (used by most clinics) often misses the mark. It gives you a snapshot, not the full picture.
For deeper insights, more advanced testing methods include:
- Four-point saliva testing: Saliva samples taken at four key points during the day
- 24-hour dried urine testing: Urine collected over a full day to track cortisol and related hormones
- Biosensor-based testing: Wearable tech that monitors real-time changes without the need for a lab
These tests track your cortisol curve, helping you spot patterns like:
- Low morning cortisol (linked to fatigue and brain fog)
- High evening cortisol (which can disrupt your sleep)
- Flatlined levels (a common sign of burnout)
If you’ve been looking into “adrenal fatigue testing”, this is usually what people mean. While “adrenal fatigue” isn’t a recognised diagnosis, the symptoms (low energy, poor sleep, brain fog) are real. In many cases, they point back to cortisol.
Cortisol and your long-term health
Cortisol is helpful in the short term, but when it stays high for too long, it can start to take a toll on your long-term health.
Research links chronic high cortisol to:
- Insulin resistance
- Higher risk of type 2 diabetes
- Weight gain around the middle
- Mood issues and increased inflammation
These effects tend to show up more in midlife, when oestrogen levels fluctuate throughout perimenopause and your body becomes more sensitive to blood sugar spikes. That’s why understanding your stress response isn’t just about getting your cycle in sync; it’s about protecting your overall, long-term health, too.
No, you don’t need a cortisol detox
Cortisol isn’t a toxin; it’s a hormone your body needs to function. The goal isn’t to get rid of it, but to keep the curve in balance: high in the morning, low at night, and responsive to real stress (not email pings or doomscrolling).
There’s no supplement, powder or cleanse that can “detox” your cortisol. But the science suggests lifestyle changes can help support a healthier rhythm:
1. Sleep like it (really) matters
Poor sleep raises cortisol, while high cortisol messes with your sleep. Getting consistent, high-quality rest helps regulate your hormonal rhythm and keeps your cortisol curve in check.
2. Move in ways you enjoy
Exercise temporarily raises cortisol (and that’s totally normal). But regular movement lowers your baseline levels over time and helps your body respond better to stress. Whatever type of exercise you prefer, consistency is what matters.
3. Fuel your body well
Balanced meals with complex carbs, healthy fats, and protein help stabilise blood sugar and support a steadier cortisol response. In one small study, increasing whole-food carbs lowered cortisol reactivity over 8 weeks, no crash diets needed. Omega-3s may also help regulate cortisol and mood – think oily fish, nuts and seeds.
4. Calm your nervous system
Mind-body practices like breathwork, meditation, and mindfulness are all proven ways to lower cortisol and reduce stress. Even if it’s just spending time outside, talking to a loved one or cuddling a pet, taking time out of your day to focus on calmness can go a long way.
What about supplements?
Some herbs like ashwagandha may help support cortisol balance, but the evidence is mixed. They can also interact with other medications and aren’t suitable for everyone (especially during pregnancy), so it’s important to check with your doctor first.
Need answers? Daye can help
Low energy, irregular periods, or mood swings? These could be signs your hormones are out of sync.
Daye’s Hormone Test is pain-free, needle-free, and checks key markers like oestradiol, LH, FSH, prolactin, and TSH. While it doesn’t test for cortisol, it can help you rule out other common imbalances and build a clearer picture of what’s going on. Designed by medical experts and processed in UKAS-accredited labs, it’s data you can trust and use to take the next step.
Cortisol isn’t the enemy; it’s essential. But when stress becomes constant, your whole system can fall out of sync. Understanding your key hormones is the first step to getting back in balance and feeling more like yourself again.
Relevant Products